In the News
-
15 Feb
As a patient, but also as a consultant with trainees, the last thing we want to think about is a doctor's inexperience while performing medical procedures....
-
31 Jan
In the following, I aim to summarise my notes from Hyderabad. The text presents an absolutely independent viewpoint, written as a personal reflection...
-
15 Jan
Blimey, in just two short weeks, Hyderabad will be at the forefront of interventional bronchoscopy in India and I couldn't be more chuffed to be...
-
23 Dec
Also known as video-assisted thoracic surgery (VATS), thoracoscopy is a minimally invasive surgical procedure that is used to diagnose and treat...
-
20 Dec
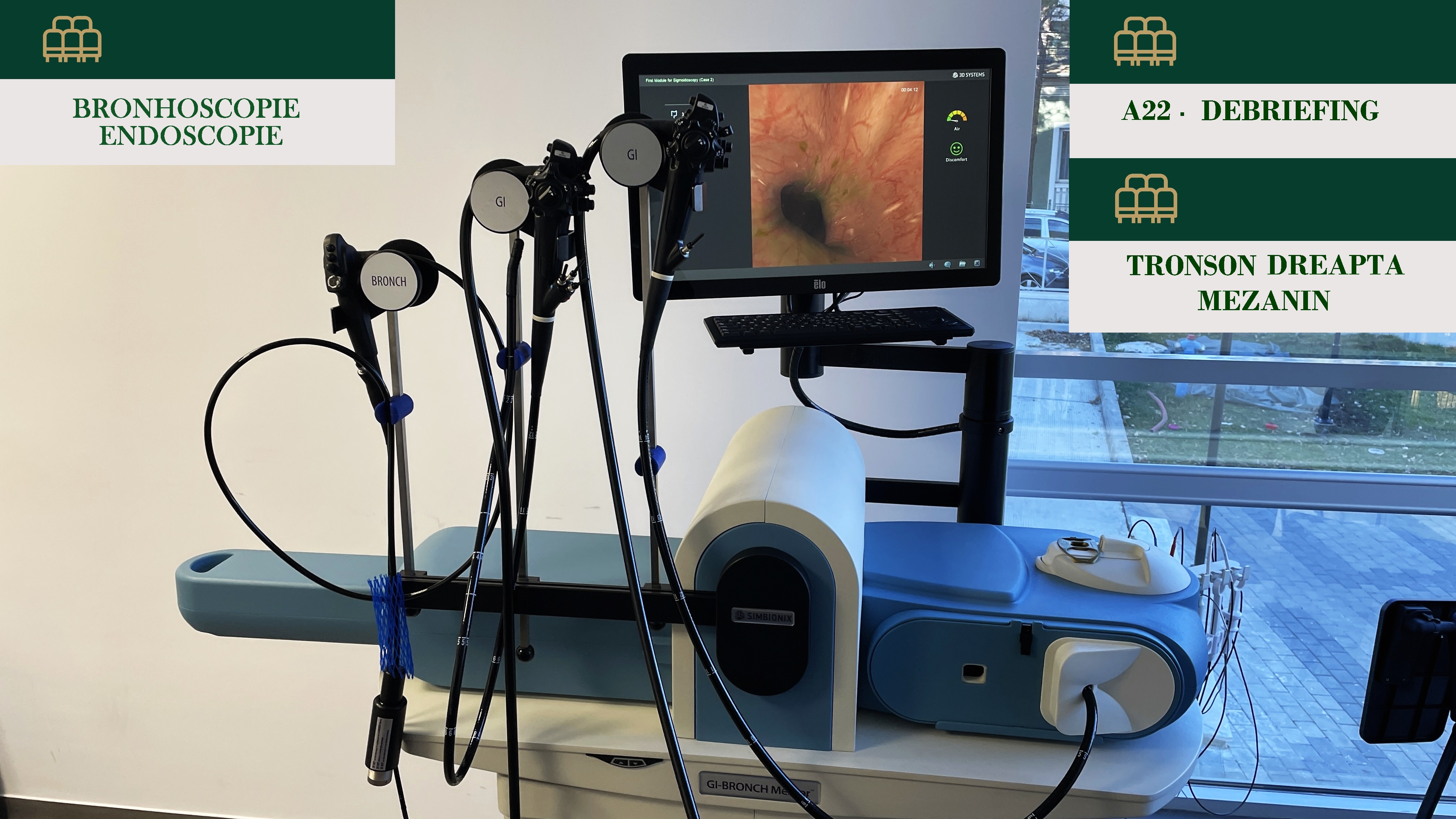
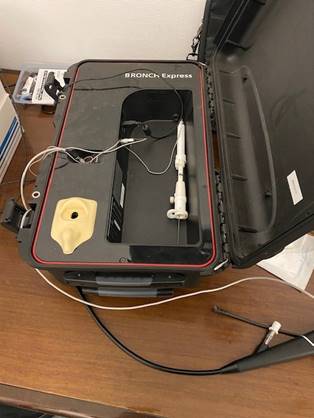
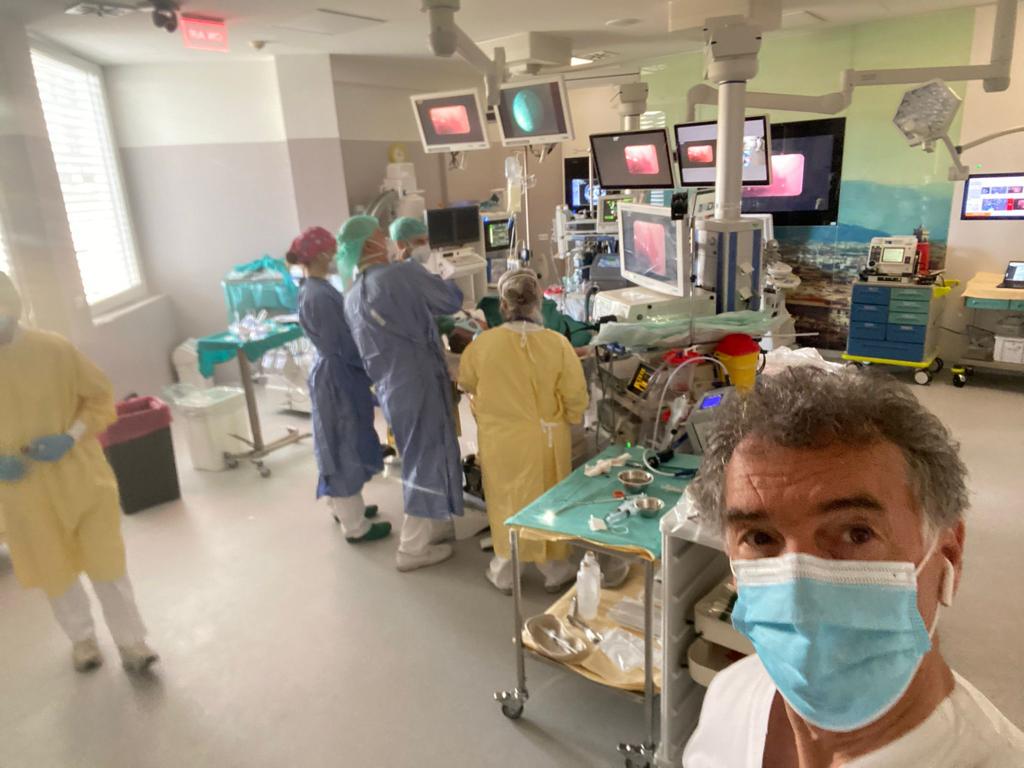
Bronchoscopy is a medical procedure that involves using a thin, flexible tube with a light and camera attached to it to view the inside of the airways....
-
15 Dec
Bronchoscopy is a medical procedure that is used to diagnose and treat various respiratory conditions, that involves inserting a thin, flexible...
-
3 Dec
Thoracic ultrasound, also known as chest ultrasound, is a diagnostic imaging technique that uses high-frequency sound waves to produce detailed...
-
8 Nov
Pleural drains, also known as thoracentesis or chest tubes, are medical devices used to remove fluid or air from the pleural space, which is the...
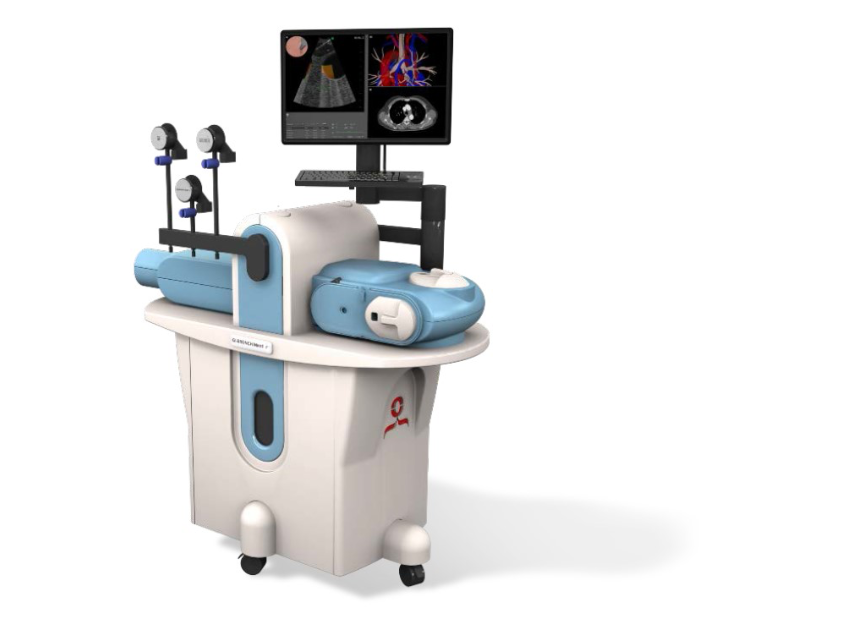
Suggested Simulators
An Online European Directory for Interventional Pulmonology (IP) Simulators, Service & Training
Europe has many centres which perform interventional procedures (IP) and can offer a variety of training opportunities. These centres have a diverse type of equipment for simulation and can offer individual opportunities for fellowships or periods of training and activities on their simulators.
Hospital with a newly appointed doctor, may require this doctor to have more time on an EBUS simulator to either confirm competency or improve capability, but can have difficulty in offering training if the institution does not have the equipment. The absence of a centralised database for simulators may limit service development of new IP procedures. On the other hand many institutions may have invested large budgets in simulators, but these remain underused outside course activity for a long period of time as there is no possibility for outside doctors to access them.
The creation of a central European IP directory of simulators, services and training might connect better the demand for simulators with the supply already available. It may easily suggest some training options close to a doctor’s home, with information about conditions for accessing simulators, or conditions for taking part in local courses or training fellowships.
The IP training in Europe is currently fragmented and not standardised. The availability of a central database of IP services and training can also offer important information on the differences between countries and can contribute to a future standardization of the training programmes that can be adopted by organisations, such as EABIP.
All participants in the project will be acknowledged, and the simulation centres will be able to promote their services through the platform and benefit through an increased utilisation of their simulators and other additional training that might be offered.
The project is a privately funded initiative with the support of EABIP (European Association of Bronchoscopy and Interventional Pulmonology).